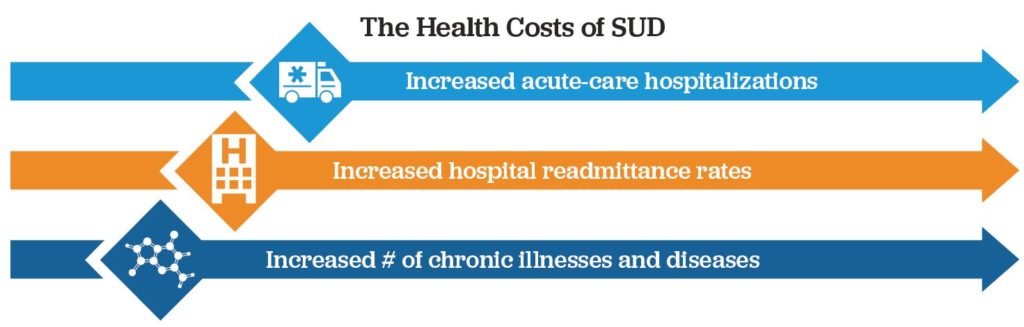
People with SUD and other mental health diagnoses account for 60% of all healthcare spending, with just 7% of the spending attributed to mental health services and 53% attributed to physical health. [1,2] SUD-related physical health issues include emergency department visits, HIV or HEP-C treatments, repeat heart valve replacements, and neonatal abstinence syndrome, among others. If people with SUD avoid new use events, they are also more likely to avoid expensive medical interventions.
Despite the connection between substance use and costly medical events, this population faces an uphill struggle to obtain much needed care. While mental health treatment has experienced meaningful advancements in the recent past, it lags physical health by decades. The stigma of mental health treatment remains a hurdle for patients, providers, and payers. For example, would we ever ask an orthopedic to treat a fracture absent a confirmatory X-ray, a cardiologist to treat hypertension absent a blood pressure cuff, or an endocrinologist to treat diabetes absent a glucose monitor? Why do we ask addiction medicine to treat SUD absent objective diagnostic information? The stigma of SUD combined with limited funding for mental health treatment discourages advancements in treatment needed to exceed subpar outcomes. For example, we would never accept curing just 1 of 5 cancer patients. Why do we accept worse for SUD treatment? True, SUD treatment funding made progress with the 2008 Mental Health Parity Act and the 2010 Affordable Care Act, yet funding and acceptance of mental health continues to fall materially short. With mental health parity, do we limit the number of blood tests that dialysis patients may have, or during cancer therapy?
More recently, the COVID-19 pandemic has exacerbated basic health-related needs, causing anxiety over employment, transportation, housing, food, social support, and basic safety. These health concerns combined with social isolation are taking a toll on people’s well-being. The Office of National Drug Control Policy reports that the thirty day rolling mean comparison of 2019 to 2020 for January to April shows that fatal overdoses increased 11.4% and non-fatal overdoses increased 18.6%. [4] SUD monitoring via random drug testing, not only helps to prevent costly medical events, but it also provides therapeutic benefits that:
- Guide therapy provided to the patient;
- Inform on patient progress or lack thereof;
- Allow for early, pre-relapse intervention via predictive analytics;
- Aid in motivational counseling;
- Help the patient develop coping and refusal skills to new use;
- Foster daily engagement in the treatment and recovery process;
- Enable contingency management;
- Promote prosocial behavior and activity;
- Enable positive affirmations and reinforcement key to mitigating future discounting; and
- Interrupt the behavior cycle of prompt, craving, preparation, and new use.
1. McKinsey & Company, April 2020: Returning to Resilience: The impact of COVID-19 on mental health and substance use (https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/returning-to-resilience-the-impact-of-covid-19-on-behavioral-health)
2. Medicare FFS Limited Data Set from the Centers for Medicare & Medicaid Services, deidentified Medicaid data, and the International Business Machines Corporation’s Truven MarketScan Commercial Database.
3. Office of National Drug Control Policy: 47097f1eea78.pdf